Telemedicine Reimbursement:
Will I get reimbursed for telemedicine?
It depends. Telemedicine reimbursement is not definitive, it varies by location, services provided, and payers.
Does health insurance cover telemedicine?
Currently, there is no set standard for private health insurance providers regarding telemedicine. Some insurance companies recognize the value of telemedicine and pay for it, whereas others aren’t quite there yet. For insurance companies which lack telemedicine reimbursement policies, prior approval is often needing before telemedicine will be reimbursed.
Fortunately, some states have parity laws that require insurance companies to reimburse at the same rate as in-person care for services provided.
Telemedicine Parity Laws
When a state enacts a telemedicine parity law, private payers in that state are required to reimburse for telemedicine coverage in the same manner as they do with in-person care. As a result, if a new parity rule is implemented, it is a major victory for telemedicine.
Numerous private payers want to cover telemedicine in either case. They are simply not legally obligated to reimburse. 29 states have now enacted parity legislation, with eight new states considering such legislation. Furthermore, because of the cost benefits that telemedicine can provide, commercial payers are becoming increasingly driven to cover it.
Although all states with telehealth parity legislation require payers to cover live video telemedicine, only a few require payers to cover store-and-forward telemedicine. Additionally, some parity statutes have unique limitations and exclusions.
States with telemedicine parity laws:
- Alaska
- Arizona
- Arkansas
- California
- Colorado
- Connecticut
- Delaware
- District of Columbia
- Georgia
- Hawaii
- Indiana
- Kentucky
- Louisiana
- Maine
- Maryland
- Michigan
- Minnesota
- Mississippi
- Missouri
- Montana
- Nevada
- New Hampshire
- New Mexico
- New York
- Oklahoma
- Oregon
- Rhode Island
- Tennessee
- Texas
- Vermont
- Virginia
- Washington
States without telemedicine parity laws:
- Alabama
- Florida
- Idaho
- Illinois*
- Iowa*
- Kansas
- Massachusetts
- Nebraska
- New Jersey*
- North Carolina*
- North Dakota
- Ohio*
- Pennsylvania*
- South Carolina
- South Dakota
- Utah
- West Virginia
- Wisconsin
- Wyoming
- *Proposed legislation to change law.
Go to the ATA website ATA website to learn more and get the latest updates.
Does medicare or medicaid cover telemedicine?
In general, Medicare Fee-For-Service Program will cover from originating sites to individuals who live in a rural geographical location, Health Professional Shortage Area (HPSA) or a county outside a metropolitan statistical area. If eligible, Medicare will reimburse for services that are “face-to-face” with the patient through telemedicine.
Telemedicine in Medicaid is covered in 48 states. Telemedicine services covered include: real-time communication, store-and-forward technology, remote patient monitoring, and a newly developing focus on mhealth (mobile health), for health education and other services. Medicare Payment Rules
In general, office and other outpatient services are covered under CPT codes 99201-99215 for Medicaid and Medicare.
In order for clinical services or an (encounter) to be covered by Medicare services need to be provided by one of the following health care professionals:
- Physician
- Nurse practitioner (NP)
- Physician assistants (PA)
- Nurse-midwives
- Clinical nurse specialists (CNS)
- Certified registered nurse anesthetists
- Clinical psychologists
- Clinical social workers
Can telemedicine be used with global reimbursements?
Yes! Global reimbursements are single payment to a healthcare provider to cover all services related to a condition or event, such as surgery or childbirth. With global reimbursement, the health care provider has the flexibility to decide how they deliver their services, allowing them to use telemedicine when appropriate. Therefore, telemedicine is a great way save the clinic money by reducing operating costs for delivering in-person medical services.
Patients can self-pay for telemedicine
With self-paying patients, they can pay for any service they want, even if delivered via telemedicine. Often patients are willing to pay out of pocket for the convenience of receiving care by telemedicine. Of note, Doxy.me Professional and Clinic accounts allow you to collect payments from patients during a telemedicine session.
Doxy.me provides free and low-cost telemedicine solutions, allowing you to reduce your overhead expenses. Start saving money and sign up for your free telemedicine account today!
Telemedicine Billing
Telemedicine is covered by many of the main commercial health insurance companies such as Aetna, Cigna, Blue Cross Blue Shield, Humana, and United Healthcare. Medicare also includes telemedicine, and the telehealth regulations have increased with the latest coronavirus epidemic. What was prohibited last week is now permitted this week. Insurance providers and Medicare are constantly reviewing and modifying their telemedicine plans.
Summary of Medicare Telemedicine Services
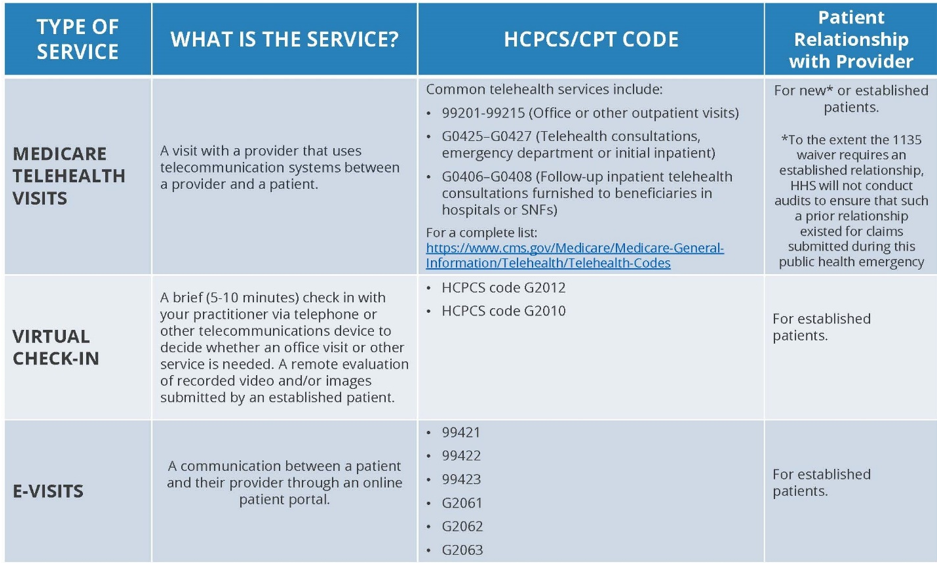
CPT Codes from CMS.gov
How to check whether the patient’s insurer supports telemedicine
Calling and verifying coverage for the patient’s insurer before their first telemedicine appointment is the easiest way to guarantee you can charge and get paid for telemedicine. Although this requires some effort, you just need to do it once for each policy. If you keep track of the call reference amount, you can use it to appeal a denied claim later. If the payer stated on the phone that telemedicine is covered and you have the call’s reference number, they must respect the claim.
Calling and asking the correct questions is the simplest way to understand what the payer requires for telemedicine. Here are some questions you can ask:
- Which healthcare providers are qualified to bill for telemedicine services?
- Are there any limitations or requirements that must be fulfilled before a patient is qualified for telemedicine?
- What types of healthcare services are available through telemedicine?
- Is there a limit on the amount of telemedicine appointments a patient may have in a given year?
- Do you cover live video telemedicine in particular?
Certain payers may provide concrete responses to these concerns that define their coverage in telemedicine. Others can simply state that they cover telemedicine for specific providers and place little restrictions on it. Since these rules differ from payer to payer and state to state, make sure to contact the payer and get their feedback. Because the regulations adjust often, the insurance company representatives may not even be informed of all the updates. Don’t be alarmed if your telemedicine claims are rejected at first; this is why we recorded the call reference number.
How and when to use CPT codes and GT/95 modifiers
The majority of payers advise providers paying for telemedicine to use the correct evaluative and management CPT codes (99201–05, 99211-15) in conjunction with a GT or 95 modifier. There is a lengthy range of Medicare codes that can care of all the qualifying health conditions, though private insurers might be looking for the specific telemedicine code: 99444. It differs according to the payer and the state in which you reside. The GT modifier informs the insurance company or Medicare that a medical treatment was provided by a telemedicine practitioner. Medicare needs a GT modifier in accordance with the correct CPT code. After charging telemedicine services, practitioners must use the CPT code with the place of service code 02, as well as a GT or 95 modifier.
How to bill telehealth facility fees
A facility fee is charged to the nearby healthcare facility that hosts the patient during the telemedicine consultation. In the new Medicare telemedicine model, for example, a patient may first visit a qualifying origin location before beginning a telemedicine visit with a medical practitioner at a different site. The origin site will charge a facility fee to offset the costs of conducting the visit. To bill for the facility fee, use HCPCS code Q3014. Research the HCPCS code for complete information regarding the facility fee.
Learn about Telemedicine
- What is Telemedicine?
- Learn more
- Advantages of Telemedicine
- Learn more
- Telemedicine Reimbursement
- Learn more
- Telemedicine Services
- Learn more
- Professional Associations
- Learn more
- Inside Telemedicine Blog
- Learn more